Our editors independently select these products. Making a purchase through our links may earn Well+Good a commission
No two groups seem to be as polar opposite as feminists and tradwives—that is, the “traditional wives” of social media who tend to preach submissiveness in marriage and that “a woman’s place is in the home.” But oddly enough, the two camps have lately collided at an uncanny meeting point: childbirth. And more specifically, unmedicated childbirth.
On both sides, there’s an empowered vision of childbirth that seems to revere a woman’s ability to harness her pain rather than dulling it with medication as she brings new life into the world. Eschewing epidurals—or anesthetics that partially or fully numb you from the waist down—is a hallmark of this vision.
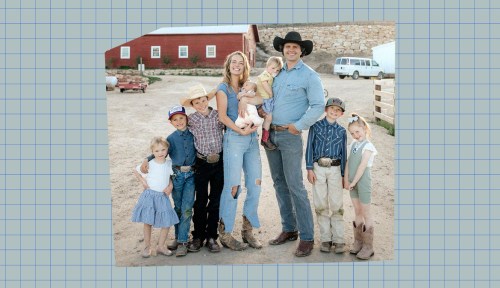
The epidural specifically was thrown into the spotlight recently after The Sunday Times published a profile of mom-of-eight Hannah Neeleman, aka Instagram user @ballerinafarm, that dubs her the “queen of the tradwives.” Neeleman, who boasts over 9 million followers, gained mainstream notoriety earlier this year when she competed in a beauty pageant 12 days after the birth of her youngest child. In the more recent profile, she talks about her preference for giving birth at home, sans pain medication. “I don’t know, I just have never loved taking it,” she tells the SundayTimes.
And she’s far from the only one taking this stance.
Behind the epidural backlash
As of CDC data from 2008 (the most recent data available), 60 percent of people who give birth get epidurals. However, so-called “natural births”—vaginal deliveries without the anesthetic—have been on the rise for the past two decades, according to Rachel Somerstein, author of Invisible Labor: The Untold Story of the Cesarean Section. As Somerstein writes in The Guardian, criticism of how the medical industry profits from Cesarean sections and epidurals along with the rising number of potentially not-medically-necessary C-sections resulted in an increase in home births assisted by midwives and doulas in the 2000s that grew even larger during the pandemic.
The idea that you can have a choice in how you give birth—in a hospital or at home, medicated or unmedicated—has been a boon for women’s agency. But that empowerment has lately come up against the rising tide of birth content on social media1. Today, there are more than 700,000 Instagram posts tagged #naturalbirth or similar. Tradwives like Neeleman, with apparently conservative values, alongside the more liberal Goop set aim for a “good birth” powered by their birth plans and their own female ferocity—that they then later share proudly via Instagram reels.
This can be a beautiful goal, if it resonates with you. But many, including celebrities like Siena Miller, say it puts pressure on women to have an idealized birth that just may not be possible based on personal medical circumstances.
Like the misguided backlash against hormonal birth control, an epidural backlash is brewing, at least among those privileged enough to have ready access to this form of pain medication. But how did unmedicated labor and delivery become the north star of childbirth?
As Somerstein catalogs, childbearing people became eager for pain medication as soon as it became available. And there’s been piles of proof through the years that epidurals specifically are safe. Indeed, Emily Oster’s 2013 pregnancy bible Expecting Better deep dives into the pros and cons of epidurals and finds there’s no evidence they negatively impact the baby (no, data does not support that epidurals can cause autism or make babies lethargic enough to have a harder time learning to breastfeed). The biggest cons are that pushing (not overall labor time) might be 15 minutes longer on average, and that the likelihood is higher for an intervention like forceps or the use of the synthetic hormone pitocin (often used to strengthen or speed up labor contractions).
Pros include reduced instances of serious medical complications like heart attacks, a recent study2 of more than 500,000 women showed. But the most obvious pro, of course, is reduced pain. Yet that seems to be somehow less of a “pro” as of late.
Part of the reason why may stem from some mid-20th-century obstetrics and midwifery philosophies that say the fear and desire to avoid pain associated with childbirth is an invention of Western medicine and that pain is something we don’t have to turn away from. Instead, pain is the sign that your cervix is dilating, that your body is doing what it’s supposed to be doing. It’s what lets you know it’s time to push. This philosophy has taken hold in birthing methods like hypnobirthing, of which Meghan Markle is a rumored practitioner.
Additionally, in today’s wellness landscape, we vaunt the idea of “being in tune with your body.” So it makes sense that something that literally numbs you out might feel icky to some at this current moment. Birth is a sacred part of life. Why wouldn’t you want to experience it wholly?
Why I loved my epidural (even as I feel the need to defend it)
At this point, it may not come as a shock to you: I had an epidural. “I loved it,” I say, chin raised, whenever I’m asked (which is weirdly often). But there’s also a nagging part of me that feels like it was a cop-out, like I’m weaker than people who white-knuckled it at home or in the hospital. Like my birth wasn’t as Good as the births of people who didn’t break down in tears from the sheer relief I experienced after the (painful) spinal shot was administered.
As my epidural started to register in my body and mind, I found myself alone in my hospital room for the first time in 10 hours since my water had unexpectedly broken six weeks early and my husband and I had driven to the hospital at midnight. I started to cry, my chest heaving, tears streaming and cries turning to sobs. My flabbergasted nurse walked in and asked what was wrong—was the epidural not working? No, I was just finally processing everything that had happened over the course of the long night. The shock of my water breaking. The 10-hour limbo of not knowing whether I was actually going to try to deliver this early. The sharp, skin-crawling, muscle-aching stabs of my contractions in my stomach, back, pelvis, hips, and legs (nobody told me about the legs). The fear of labor looming before me when I hadn’t expected to give birth for another six weeks. I was still supposed to be pregnant! I was not ready.
But my baby was. So over the next 24 hours, the pain relief from my epidural allowed me to make peace with, or at least inhabit, that reality. Once you have an epidural, you’re not allowed to get up from your bed because of the numbness, but I still found myself wanting, needing, to stretch and move in cat-cow and child’s pose throughout my labor as my cervix dilated. Ironically, with the pain numbed (but certainly not gone), I felt more in touch with my body after my epidural than before.
Another unexpected boon? The catheter put in post-epidural meant that for the first time in over two months, the constant feeling of having to pee was finally gone. It was like there had been some sort of uncomfortable white noise buzzing in my head that was finally silenced. Overall, after nine months of discomfort between always having to pee, feeling shaky on my legs thanks to loose joints, an alien kicking my ribs, and all the other joys of pregnancy, the rest I got on my epidural was the first time I’d felt comfortable in a really long time. Until, of course, the contractions got stronger and stronger, and it was time to push.
In short, I have no regrets about my epidural, yet my need to justify it persists. An epidural was always the plan. I am of the “why suffer with a headache when you can take a painkiller?” school of thought. Why wouldn’t this attitude extend to childbirth and an epidural? Why doesn’t “I wanted to reduce the pain of childbirth” feel like enough of an explanation these days?
Neeleman’s vague feeling that she just doesn’t like them for some nebulous reason may speak to why. The obstetrician responsible for popularizing the idea of natural childbirth, Grantly Dick-Read (a man), “asserted that by being fully conscious and emotionally present for birth, women could achieve ‘the perfection of womanhood,’” Somerstein writes. “He yoked ‘natural’—meaning unmedicated—labor to what he saw as women’s biological imperative and the ultimate expression of female identity.”
Dick-Read was just one male doctor writing in the 1950s, but the vision of the life-giving Madonna, laboring on another sacred plane of existence, seems to have a grip on the idea of a Good Birth three-quarters of a century later. As seen in her Sunday Times profile, Neeleman’s Instagram reel of her 2022 labor with baby number seven shows her blissed out in a warm glow, surrounded by children and midwife, almost sacredly at peace. A vision of domesticity and tradwifery.
Then there’s the reality that women’s pain just doesn’t rate as being important. As women who experience periods, whose medical concerns get routinely dismissed by doctors, whose debilitating and painful conditions are understudied and ignored, one would think mitigating that pain should be important to us. But societal de-prioritization is a hard thing to shake.
Or maybe it’s just that we women are accustomed to suffering. For fashion in uncomfortable heels, for muscle tone in bootcamp classes, for thinness on cleanses, for parents, spouses, and children as we shoulder the mental and physical load. Suffering is noble. You only get the chocolate cake after you’ve earned it in spin class.
Ultimately? You do you
More choice can only be good for women’s health. A home birth with no complications surrounded by family and the ability to sleep in your own bed—no wires, no beeping, no harsh lights—can be something incredible to aim for, if that’s what sounds supportive and meaningful to you. Maybe there’s another pull there: That generations of women before you have labored at home without painkillers. Maybe you want that, too.
Meanwhile, in the hospital, perhaps there are more women getting epidurals than Instagram might lead one to believe.
Neeleman herself got a taste of a less social media-ready way of laboring. She delivered two of her eight children in the hospital. For her third-youngest’s birth, Martha, Neeleman’s husband—whom the Sunday Times profile paints as domineering—was not present because of work. Martha was expected to be a large baby. So Neeleman had an epidural. “It was an amazing experience,” Neeleman tells the SundayTimes, in a whisper. “It was kinda great.”
Marsh, Anna et al. “The perfect birth: a content analysis of midwives’ posts about birth on Instagram.” BMC pregnancy and childbirth vol. 23,1 422. 7 Jun. 2023, doi:10.1186/s12884-023-05706-2
↩︎Kearns, Rachel J et al. “Epidural analgesia during labour and severe maternal morbidity: population based study.” BMJ (Clinical research ed.) vol. 385 e077190. 22 May. 2024, doi:10.1136/bmj-2023-077190
↩︎
Sign Up for Our Daily Newsletter
Get all the latest in wellness, trends, food, fitness, beauty, and more delivered right to your inbox.
Got it, you've been added to our email list.