Maybe your trigger is going out to eat. Or you get IBS flare-ups every time you’re about to lead a big presentation at work. First come the stomach pains, then you start internally freaking out (ugh, why now?!), all while trying to appear cool and composed on the outside. But deep down, you know it’s all downhill from here.
People with Irritable Bowel Syndrome (IBS) know their warning signs and symptoms (like abdominal pain, plus constipation, diarrhea, or both) all too well, but what many people don’t realize is that there are actually varying degrees of the syndrome.
“There’s a definite spectrum with IBS, and people can have cases ranging from mild, to moderate, to severe,” says Shanti Eswaran, MD, gastroenterologist and associate professor at the University of Michigan. “And where you fall on the spectrum often determines your treatment,” she adds.
A whopping 10 to 15 percent of Americans suffer from IBS, according to the American College of Gastroenterology—and it’s the most common disease diagnosed by gastroenterologists. Dr. Eswaran predicts that the large percentage is likely due to so many people suffering from mild symptoms.
Still, no matter where you fall on the spectrum, the good news is that there are treatment options tailored to you. Keep reading to see where you might land—and how you can find some much-needed relief.
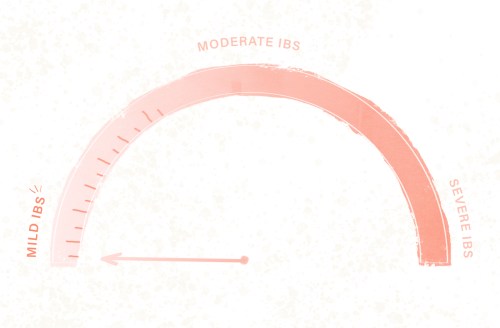
On the spectrum: Mild IBS
What’s up: Even though IBS is so prevalent in the United States (and—just great—is more common in women than men), only about 5 to 7 percent of Americans have actually been diagnosed with the syndrome. The reason for the discrepancy? “Many people with mild IBS suffer without seeking help or getting a diagnosis,” says Dr. Eswaran. Instead, she says, there’s a lot of self-diagnosis—people with mild IBS who have never sought care, for example, might call it a “nervous stomach.”
If you fall on the mild side of the spectrum, you may just deal with the symptoms. The occasional flare-ups happen, and when they do, you might have to run to the bathroom more frequently. And yes, the diarrhea or constipation is frustrating, and the stomach pain can hurt, but on this side, the symptoms aren’t debilitating.
Treatment: IBS shouldn’t be something you just have to “tough out.” You’ll want to see a doctor, because there are better options than just putting up with the pain and annoyance. (A doctor can also help rule out any other potential issues like endometriosis or inflammatory bowel disease.)
The good news? “First-line treatments are typically not medicine,” says Neilanjan Nandi, MD, gastroenterologist, assistant professor and director of the Center for Inflammatory Bowel Diseases at Drexel University College of Medicine.
Instead, your doctor will explain that your symptoms are real, and talk about the lifestyle treatments that can make a difference, adds Dr. Eswaran. For example, your doctor might suggest dietary changes, like avoiding dairy for a week or so, as well as alcohol and fried, fatty foods. Coffee and IBS don’t mix well, either: Caffeine is a stimulant, and stimulants, well, make you want to poop. These might not be triggers for everyone with IBS, but a short trial can help you figure out if it’s personally a problem.
Other suggestions your doctor may have: getting regular exercise, practicing stress management (through yoga or meditation), and putting yourself on a routine sleep schedule. “People might know that trying out a new medication or a highly stressful event could trigger their IBS, but many patients don’t realize that sleep is also tied to IBS symptoms,” says Dr. Eswaran. In fact, so important is a regular sleep schedule that one study published in the American Journal of Gastroenterology found that nurses who worked rotating day and night shifts had an increased risk of developing IBS, compared to those who just worked a typical day-time schedule.
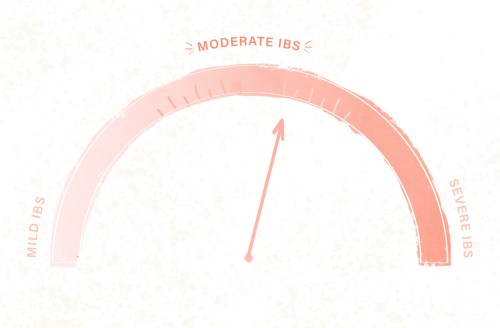
On the spectrum: Moderate IBS
What’s up: If you fall more in the middle of the spectrum, your symptoms really start impacting your quality of life and routine. Some people in this group avoid eating during a flare-up, while others with moderate IBS may even need to work from home on their worst days.
If earlier lifestyle changes didn’t help (though doctors encourage you to keep things like exercise and meditation up), and symptoms seem more frequent or they’re getting worse, it’s important to go back to your doctor for other potential treatment options.
Treatment: Your plan of attack: Work with your doctor to figure out what’s driving your symptoms—sometimes it’s food-related. For other people it might be more anxiety-related. “If anxiety is triggering your IBS, your doctor might refer you to a psychologist or psychiatrist who can talk about the GI stress cycle, and help you with anxiety management,” says Dr. Eswaran.
So what’s the GI stress cycle? Our guts are closely connected to our minds, so anxiety over IBS symptoms can actually make the problem worse. It’s why, for example, when you start to think nervous thoughts in your head, you might then begin to feel “butterflies” in your stomach. Research even shows that patients who suffer from anxiety or depression also have a higher prevalence of IBS.
“Sometimes if you can treat the anxiety, you can help a person’s GI symptoms as well,” says Dr. Eswaran. Cognitive behavioral therapy, deep breathing techniques or even hypnotherapy have all been shown to help people with IBS, says Dr. Nandi. “The challenge is finding a therapist who is interested in IBS and able to work with you—plus, insurance may not cover your sessions,” Dr. Nandi adds.
Another challenge: “This route takes a lot of effort and motivation on the patient’s part, and they must willingly accept therapy as a GI treatment,” says Dr. Eswaran. “Many people come in and just want treatment for the physical symptoms, and not the emotional ones,” she adds. But therapy actually gives you long-lasting positive effects.
You may also come out of the appointment with a prescription for anti-anxiety or antidepressants to treat your IBS. For example, tricyclic antidepressants can help with potential depression symptoms, but at the same time can block the activity of neurons that control the intestines to help reduce pain.
As for dietary changes, a doctor might suggest people with moderate IBS work with a dietitian, and go on the low-FODMAP diet. FODMAPs, specifically, are short-chain carbohydrates that for some don’t get absorbed properly in the gut. The goal is to figure out which of these carbohydrates may set off your IBS symptoms. (For example, some people could have flare-ups after eating legumes and apples, while for others it’s garlic and wheat.) First, you cut out all FODMAPs, then slowly start adding them back one at a time, to see what may be a trigger.
“The diet is restrictive—so it’s not recommended for people who fall on the mild end of the spectrum—but it’s evidence-based, and can really help with the pain and bloating that comes with IBS,” says Dr. Eswaran, who herself has done research on the diet.
And for extra help, consider trying peppermint oil, a well-established natural remedy to help mild to moderate IBS, says Dr. Eswaran.
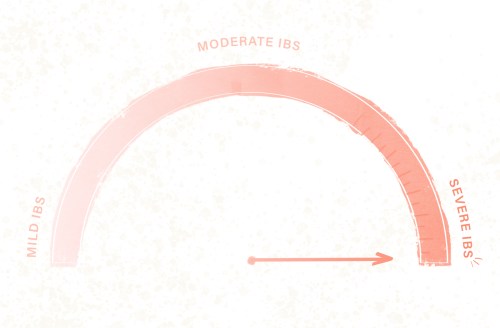
On the spectrum: Severe IBS
What’s up: People who land here likely have a lot more abdominal pain, to the point where it’s debilitating and drastically affecting their quality of life. “The pain is interfering with your personal relationships, and may even keep you from working,” adds Dr. Eswaran.
What’s surprising: “The people with the most severe cases of IBS often have a history of trauma or abuse, like a sexual abuse or assault, or witnessing a domestic violence at an early age,” says Dr. Eswaran. “Their mind-gut interaction has been seriously affected,” she adds.
Treatment: If you fall along this far end of the spectrum (and assuming everything from colon cancer to gallstones has been ruled out), doctors will likely suggest anti-anxiety or anti-depression medication along with regular visits to a psychologist for cognitive behavioral therapy. A diet issue has likely been ruled out by this point, but if you haven’t tried a low-FODMAP diet yet, your doctor may want you to. Your doctor will also likely prescribe you medication to deal with the symptoms, such as one only for women with IBS who have severe diarrhea, or another to decrease bacterial overgrowth when over-the-counter treatments don’t work.
Doctors, though, encourage people at this end of the spectrum to not just rely on these pills because they won’t solve all your issues—plus some can come along with side effects. “At this point, you’re dealing with so much more than just the physical symptoms,” says Dr. Eswaran, which is why it’s so important to understand the mind-gut connection, and why therapy really matters.
Sign Up for Our Daily Newsletter
Get all the latest in wellness, trends, food, fitness, beauty, and more delivered right to your inbox.
Got it, you've been added to our email list.











